Although breast cancer has been a human illness for thousands of years, ductal carcinoma in situ or DCIS (also known as intraductal carcinoma) is a relatively new diagnosis, and we are learning more about it all the time. Until mammography became a routine part of medical care, we didn’t see much DCIS. Now, we do. Approximately 24% of all new breast cancers diagnosed in the United States in 2002 were DCIS.
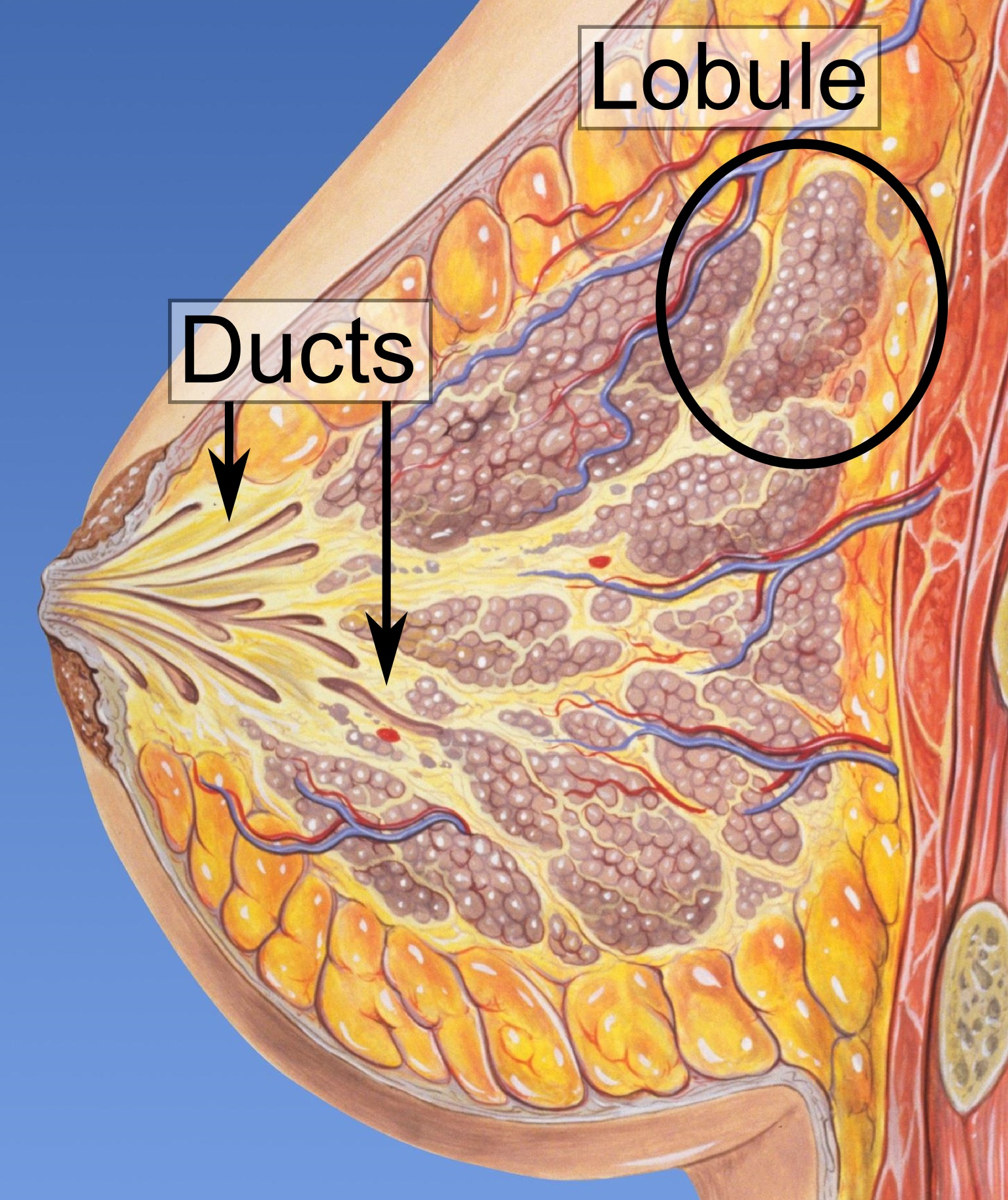
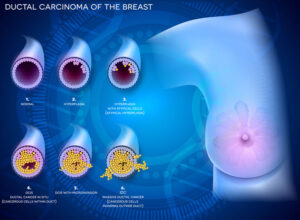
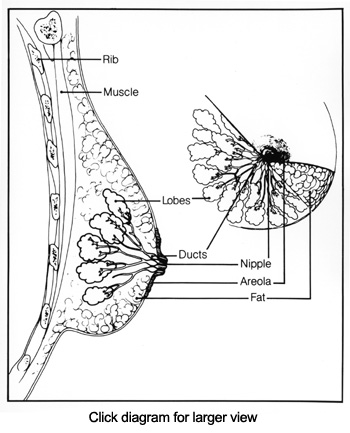
Most breast cancers (carcinomas) arise in cells that line the ducts and lobules of the breast. We still don’t know what happens exactly, but for some reason, the cells start growing when they are not supposed to be growing. When cells in the lining of breast ducts are growing inappropriately, this is called hyperplasia; when they grow inappropriately and do not appear normal under the microscope, they are called atypical.
DCIS is a term used to describe cells that are growing inappropriately inside the ducts of the breast (see diagram) and look like cancer cells under the microscope. These abnormal cells have not spread into the surrounding fatty breast tissue or to any other part of the body.
Some cell changes are important, while others are less important. DCIS cells lack the biological capacity to metastasize or spread elsewhere in the body as cancer cells do. So why do DCIS cells fall into the category of cancer cells?
Some DCIS cells can change genetically and become true cancers, and women should not be lulled into thinking that a DCIS diagnosis can be ignored or dismissed. We still do not know for sure which DCIS cells will change and become invasive and which will remain DCIS. It is probably most useful to view a diagnosis of DCIS as an indication that a woman has a greater risk of developing breast cancer, especially if she receives no treatment for the DCIS.
Cancer is an illness that needs extra care in these COVID days because if you get COVID along with cancer it’s very dangerous, you must test yourself against covid after every few days with Covid self-testing kits, which are also known as rapid antigen test kits.
There are different kinds of DCIS. It is important for the individual who is diagnosed with DCIS to know how aggressive or risky her cell type is. For example, comedo is considered more aggressive (high-grade) than cribriform (low-grade). This information is part of an accurate diagnosis by the pathologist and helps define treatment options, which in turn affect whether DCIS becomes invasive breast cancer.
A diagnosis of DCIS depends on the pathologist, and the diagnosis may be controversial. Therefore, second opinions may be important. If a woman seeks a second opinion, she needs to take her slides and blocks that contain samples of the cells taken during her biopsy to another pathologist, and she must be prepared to pay for this additional opinion.
People often fail to get a second opinion on pathology. However, if the pathology is incorrect, the treatment choices are much more likely to be incorrect and possibly ineffective as well.
You can also request second opinions for mammography, ultrasound, and treatment. If you choose to have a second opinion for mammography or ultrasound, it is important to take the original films, not copies, to the physician, and to carry them to the radiologist yourself if possible.
Whether your doctor refers to DCIS as cancer or pre-cancer, it requires careful treatment and follow-up to avoid the possibility of invasive breast cancer developing. On this Web site, we refer to DCIS as cancer.
There is a lot of research going on that will help sort out which kinds of DCIS are aggressive and how to determine optimal treatment for each kind.