What the pathologist does, doesn’t do, and should do.
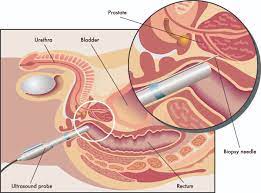
The tissue removed during the biopsy will be sent to a pathologist for review. This process may take several days or more.
It takes time to properly study a biopsy, and it should not be rushed. The pathologist examines the tissue with a special microscope to determine whether there are any cancer cells in the tissue sample or what other kinds of cells are present.
The importance of a pathology report for patients with breast disease, specifically breast cancer, DCIS, atypical hyperplasia, and other benign findings is that it helps determine what course of action is needed, including treatment and follow-up.
If your pathology report is inaccurate, your treatment may not be appropriate.
A pathology report is a formal description and conclusion regarding the tissue that has been removed during the biopsy. The report usually has three parts:
- A gross (obvious) description of the tissue samples, including the size, dimension and weight of each, and how the tissue was preserved by the pathology lab and sliced thin for examination under the microscope
- A description of what the pathologist sees on microscopic examination of the tissue
- The diagnosis, with details about the major pertinent findings present in the biopsy
A pathology report that documents DCIS should have information about the size and grade of the DCIS. The report may also document specific marker proteins present in the tumor, which may help determine a specific course of treatment (for example, hormone therapy).
DCIS is divided into different subtypes: the comedo, cribriform, micropapillary, papillary, and solid. It is important for the pathologist to identify the subtype to help to determine if the lesions are likely to recur and whether they are likely to become invasive. There is no classification system that can accurately predict which subtype is likely to recur as an in situ or as invasive cancer.
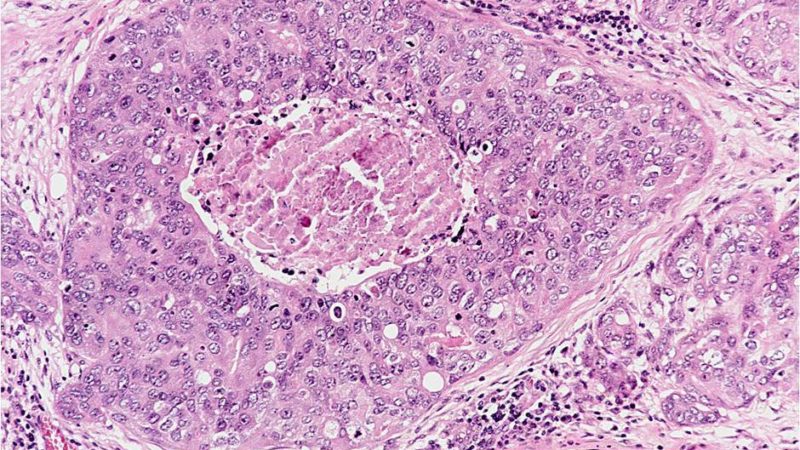
Comedo type DCIS. Comedo looks and acts differently from other in situ subtypes. Comedo tends to be slightly more aggressive than other forms of DCIS. These cells are closer to invasive breast cancer cells in how they look and behave than other forms of DCIS. Comedo cells look different under the microscope because the center of the duct is plugged with dead cellular debris, known as necrosis. Necrosis seen under a microscope in DCIS usually means that the cells are fast-growing and are generally more aggressive or high-grade. Also, microcalcifications (small abnormal calcium deposits) are frequently seen in the areas of necrosis.
Cribiform. These cells do not completely fill the ducts. The pattern has little holes and slits.
Micropapillary and papillary. These two types have fern-like projections of cells into the center of the duct. The micropapillary type projections are smaller than the papillary type.
There are three factors that are most important in determining what the DCIS cells are likely to do. These are:
- The extent of disease in the breast, or the size of the DCIS as measured by the pathologist.
- The status of the margins of the biopsy tissue.
- The grade of the DCIS.
The margins are important for treatment decisions — for example, surgery, radiation therapy and/or hormone therapy. Of the three pathology factors, the most important, uncorrected for margins, is grade. Grade is important for prognosis (prediction of probable outcome). Grading looks at the structure of the cancerous cells and their growth patterns.
Histologic grade refers to how much the tumor cells resemble normal cells (called differentiation). The lower the grade, the more the cells resemble normal cells. DCIS and low-grade tumors grow relatively slowly. High-grade tumors, in contrast, are thought to grow rapidly, and in the case of DCIS, are more likely to lead to invasive cancer in the future.
Nuclear grade refers to the rate at which the cells are dividing to form more cells (called proliferation). Cancer cells that divide more often are faster growing and more aggressive than those that divide less often. The nuclear grade is determined by the percentage of cells that are dividing. Cells have different grades ranging from 1 to 3.
Remember, the lower the grade, the more normal the cell. While high-grade DCIS is more likely to become an invasive cancer, it is also the easiest to contain. It tends to grow in a continuous pattern within the duct and is more localized within the breast. Low grade lesions tend to have more gaps and can be more widespread.
The kind of cells found, the size of the DCIS lesion, the grade of the DCIS, and the extent of the removal of the mass (margins) will be important in determining treatment options.
“Clean margins” are very important in predicting local recurrence of DCIS. However, even if the margins of the biopsy are “clean,” meaning no cancer cells or DCIS cells have been found, there is no guarantee that all the problem cells have been removed. Why? Because DCIS may grow in a discontinuous way with gaps of up to one centimeter between tumor foci.
You may be asked to obtain a post-operative mammogram to be sure that all microcalcifications or the suspicious area have been removed. This mammogram should be performed as soon as the patient can tolerate breast compression. The scar forming in the breast after a biopsy may mean that additional views will need to be taken at this time. Having both the margin status and the postoperative mammogram is important in knowing if all the DCIS was removed.
Sometimes another biopsy has to be done. This is called “re-excision” and it is done to ensure that all the microcalcifications have been removed and all other tissue areas of concern are removed. Sometimes it may be done to be sure that clean margins have been achieved.
Occasionally, some invasive cancer cells are found with the DCIS cells when the tissue is examined by the pathologist. It is important to note that if any invasive cancer cells are found, the diagnosis is no longer DCIS, but invasive breast cancer. Likewise, if a woman is diagnosed with invasive breast cancer, DCIS cells are sometimes found in the sample. Again, in this case, the diagnosis is invasive breast cancer.
The degree of risk of invasive cancer following a diagnosis of DCIS depends on three things: the grade of the cells, the extent or size of the DCIS in the breast, and the length of follow-up.
Knowing the extent or size of the DCIS area is important in deciding on treatment, but it is difficult to know this exactly because DCIS usually cannot be felt and is sometimes hard to see even on a mammogram. The pathologist can sometimes estimate the extent of DCIS and will put this information in the pathology report.
DCIS, or noninvasive breast cancer (disease that stays within the milk ducts and does not spread to other parts of the body), has an excellent prognosis if properly treated.

